Freemodule
The following is a free module taken from Biofeedback Bootcamp©. The complete Bootcamp offers 14 complete modules. Sign up today!
BIOFEEDBACK
CONCEPTS
The Highway Patrol periodically places a radar speed display on residential roads. The device shows motorists how closely their speed matches the posted 20-mph limit. This speed display illustrates the concept of biofeedback: the display of information about biological activity (speed) back to an individual (a motorist) to improve performance. Defined broadly, the biological activity we feed back can be about muscle action potentials, the position of a limb, or driving speed.
Your conceptual model of biofeedback affects the way you think about biofeedback and how you define your patient’s role in training. Before you proceed, write down a paragraph that describes how you explain biofeedback to your patients.
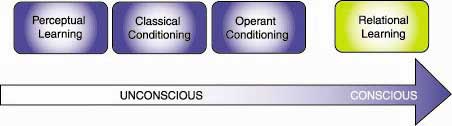
At the start of this module, we will review perceptual learning, classical and operant conditioning, and relational learning. We will examine five models that have shaped conventional beliefs about biofeedback. Next, we will study two models that emphasize skill development. Finally, we will discuss how to optimize the training process.
Students completing this module will be able to describe and explain the clinical implications of:
- definitions of biofeedback
- concepts of control in biological systems
- overview of principles of human learning as they apply to biofeedback: (a) learning theory (e.g., classical and operant conditioning, discrimination, generalization, and habituation)
- cybernetic, operant conditioning, drug, placebo, and relaxation models of biofeedback
- Blanchard and Epstein’s (1978) self-regulation model and Shellenberger and Green’s (1986) mastery model
- critical training factors including sources of biofeedback information, the social relationship between therapist and patient (including the person effect), modeling, coaching skills, patient motivation, continuous assessment, the patient’s role in treatment, practice, and bidirectional training
- voluntary control through active and passive volition
- incorporating current studies in treatment design
- personalizing treatment
- patient selection of effective self-regulation strategies
- popular biofeedback metaphors
LEARNING PROCESSES
We learn most psychophysiological responses through the unconscious processes of perceptual learning, and classical and operant conditioning, and the conscious process of relational learning.
Perceptual learning
Perceptual learning allows us to categorize stimuli and recognize that we’ve encountered them before. This learning process enables a patient to recognize that her headache is a migraine as opposed to a tension headache.
Classical conditioning
Classical conditioning prepares us to respond rapidly to future situations. Classical conditioning underlies the placebo response, which can be conceptualized as a learned healing response.
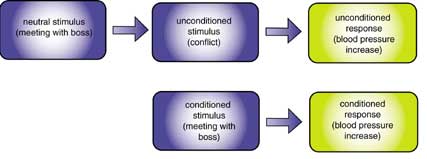
An unconditioned stimulus (conflict) elicits an unconditioned response (blood pressure increase) without learning.
Classical conditioning associates a neutral stimulus (meeting with boss) with an unconditioned stimulus (conflict). Through repeated pairing, the neutral stimulus becomes a conditioned stimulus that elicits a conditioned response (blood pressure increase). Failure of an unconditioned stimulus to follow the neutral stimulus extinguishes (weakens) a conditioned response.
Operant conditioning
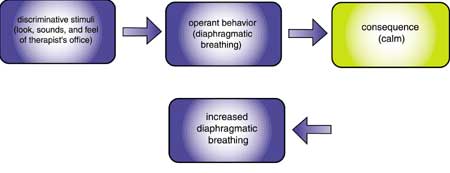
Operant conditioning adjusts behavior (operant) in response to its consequences.
A person’s actions in a situation result in consequences that may increase or decrease the likelihood of this behavior in similar situations. The identifying characteristics of a situation are called its discriminative stimuli and include how the situation looks, sounds, and feels. Discriminative stimuli tell us which consequences are operating.
In positive reinforcement, behavior (diaphragmatic breathing) is followed by a positive consequence (calm) that increases its future likelihood in situations with similar discriminative stimuli (therapist’s office).
In negative reinforcement, behavior (diaphragmatic breathing) allows the person to escape or avoid an aversive state (anxiety), thereby increasing its future likelihood in situations with similar discriminative stimuli (workplace).
In extinction, the frequency of behavior (diaphragmatic breathing) declines in a situation (workplace) when it is not reinforced (patient is unable to achieve calm).
Both classical conditioning and operant conditioning involve generalization, discrimination, and habituation.
In generalization, a person learns to respond (blood pressure increase) to stimuli that resemble the conditioned stimulus (argument with spouse) or to perform an operant behavior (diaphragmatic breathing) in situations that have different discriminative stimuli (driving during rush hour). Generalization allows us to transfer performance of self-control skills to situations outside a therapist’s office like home and the workplace.
In discrimination, a person learns to ignore stimuli that differ from the conditioned stimulus (not react to an argument with spouse) or to withhold an operant behavior (diaphragmatic breathing) when the situation is inappropriate (sprinting). Discrimination insures that our behavior is appropriate to a specific situation.
In habituation, the brain ignores a constant stimulus because it provides no new information. Office workers learn to ignore the sound of an elevator so that it no longer produces a conditioned response. The color of a relaxation reminder (a plastic dot) may have to be regularly changed so a patient will not ignore it.
Relational learning
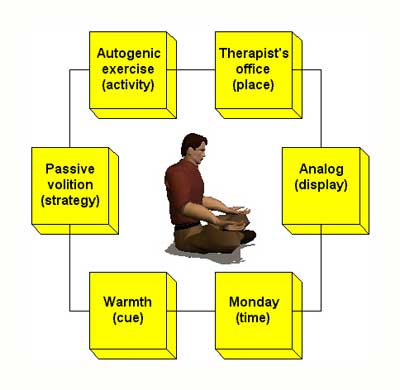
Relational learning is conscious and allows us to associate stimuli that occur at the same time. This learning process provides us with autobiographical knowledge (information about our experiences). In a clinical context, it provides conscious memories a patient can retrieve and use to guide behavior (how he warmed his hands during an autogenic exercise in his therapist’s office last week).
A relational memory of handwarming is illustrated below. The patient experienced all these elements at the same time and linked them together.
FIVE INFLUENTIAL BIOFEEDBACK MODELS
Five models have greatly influenced therapist and researcher conceptions of biofeedback. These include the cybernetic, operant conditioning, drug, placebo, and relaxation models.
Cybernetic model
The cybernetic model proposes that “biofeedback is like a thermostat.” The term, biofeedback, originated in cybernetic theory. The components of a thermostat system include a set point or goal (75 degrees), system variable or what is controlled (room temperature), negative feedback or corrective instructions (commands to change furnace output), and positive feedback or commands to continue action (commands to continue furnace output).
From the perspective of the cybernetic model, biofeedback training supplements a patient’s proprioception to bring a malfunctioning biological system variable (blood pressure) under better control.
Operant conditioning model
The operant conditioning model proposes that “biofeedback is the operant conditioning of physiological processes.” From this perspective, voluntary changes (reduced muscle bracing) are strengthened by reinforcing consequences (feedback display). This model implies that awareness of which change is being reinforced is unnecessary and disregards the instructional elements that are critical to training success.
The operant model has several problems. First, operant conditioning is only one of several learning processes involved in self-regulation training. Classical conditioning, cognitive learning, motor learning, and social learning may also be involved.
Second, reinforcement without systematic instruction is an inefficient way to teach a skill. This would be like a track coach who announced a sprinter’s time, but never demonstrated technique or corrected her form.
Drug model
The drug model asserts that “biofeedback treatment corrects symptoms like a drug.” This model is implied when a patient receives only three sessions of temperature biofeedback regardless of whether she can warm her hands to 95 degrees F on command.
The drug model is counterproductive because it places the patient in a passive role (analogous to taking aspirin) and emphasizes dosage (the number of sessions) over skill mastery. If you believe that skill mastery affects treatment outcome, then patients should be trained to criterion and not be limited to an arbitrary number of sessions.
Placebo model
Therapists using the placebo model believe that “biofeedback produces nonspecific effects, like a drug, due to patient beliefs.”
While the “laying on of electrodes” undoubtedly produces symptom improvement, this model discounts the contribution of skill learning. Second, the changes produced through biofeedback, like increased end-tidal CO2, can be very specific and are due to modified breathing mechanics instead of patient beliefs.
Relaxation model
The relaxation model views biofeedback as inherently relaxing. Based on this model, therapists may administer biofeedback without relaxation instructions and researchers may compare biofeedback to relaxation procedures like Progressive Relaxation.
This approach suffers from serious misconceptions about biofeedback. First, feedback about your physiology is not always relaxing. For example, a patient told that her blood pressure is elevated will not be calmed by this news.
Second, whether biofeedback training produces cultivated low arousal depends on relaxation instruction and the patient’s approach to learning. For example, an extreme Type A patient learning to lower EMG levels could exacerbate stress symptoms by competing against the electromyograph.
Finally, even traditional relaxation procedures like Autogenic exercises can produce distress. Relaxation-induced anxiety has been reported for up to 40% of patients receiving relaxation training.
MODELS THAT EMPHASIZE SKILL DEVELOPMENT
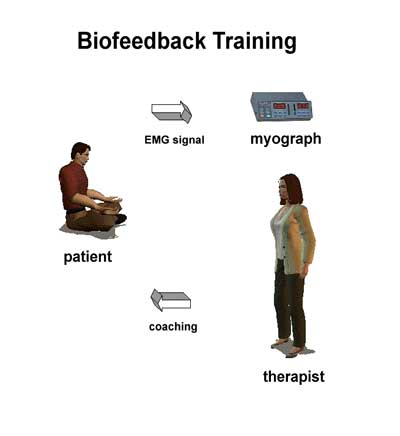
Blanchard and Epstein (1978) and Shellenberger and Green (1986) developed models of self-regulation that emphasize the mastery of self-regulation skills. These approaches are consistent with the view that biofeedback is information. From this perspective, a therapist coaches the patient to use information about her physiological performance to achieve voluntary control to reduce symptoms and promote optimal functioning.
Blanchard and Epstein’s self-regulation model
Blanchard and Epstein (1978) proposed that self-regulation consists of five components. Self-monitoring is scanning yourself in a situation (checking your breathing during a job interview). Discrimination means identifying when selfregulation skills should be used based on situational (stressful confrontation) and internal (rapid heart rate) cues.
Self-control is the use of a skill to achieve a desired state (practicing effortless breathing to lower arousal). Self-reinforcement is use of internal (self-praise) or external rewards (clothing) for use of a skill. Finally, self-maintenance is long-term skill practice which is aided by regular review.
In the context of this self-regulation model, a successful hypertension patient:
- understands hypertension and the strategy for control
- modifies risk factors (reduced saturated fat and salt intake)
- monitors symptoms (scans body several times a day for posture and breathing pattern, and charts blood pressure daily)
- practices self-control (relaxes posture, breathes effortlessly, and performs both abbreviated and deep relaxation exercises)
- rewards her self (praises her self for practice and results, and draws a connection between practice and lower medication dosage and pressure)
- maintains progress (reviews progress, modifies practice based on experience, and schedules booster sessions with a therapist as needed).
After six months practice, cues like red traffic lights and cold hands automatically trigger self-regulation responses. They become attractors. Now, a healthy lifestyle becomes rewarding and cheating becomes aversive.
Shellenberger and Green’s mastery model
Shellenberger and Green (1986) advanced a mastery model that compares biofeedback training to coaching an athletic skill. This training process is social, since you are working with another person or group, and biobehavioral, since this instruction uses behavioral principles to control biological processes.
The biofeedback training process contains these components:
- relationship with therapist
- competent therapist who has developed and models self-regulation skills
- clear training goals
- rewards for approximating goals
- sufficient time and practice for mastery
- effective instructions as part of systematic training
- feedback of information to the patient
- practice
THE TRAINING PROCESS
Mere exposure to information about our physiological performance produces no dependable effects. For example, viewing a stopwatch does not reliably improve a runner’s form.
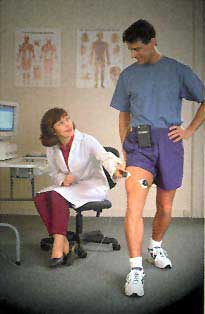
The effect of information depends on how it is used. When biofeedback is combined with physical therapy, it becomes biofeedback-assisted rehabilitation. When combined with relaxation training, it becomes biofeedback-assisted relaxation. Without rehabilitation or relaxation coaching, the information is neither rehabilitating or relaxing.
Sources of performance information
Don’t assume that biofeedback requires hardware. Information about your personal biological activity can be detected with or without hardware. Natural proprioception (bodily sensory feedback) will be your patient’s main source of information when she has learned to scan her body. Examples: touch your finger to your wrist to detect pulse rate or touch your cheek to detect hand temperature.
During training, you can supplement proprioception with high technology or low technology instruments that monitor performance. Don’t confine your concept of biofeedback to the traditional modalities like EEG, EMG, skin conductance, and temperature. While invaluable in many clinical applications, your patient may not require biomedical devices.
Peper has suggested that ordinary devices can provide valuable performance feedback. For example, facial expression during public speaking can be modified using a mirror. Balance can be improved using a pair of bathroom scales and hand tremor by a graduated set of bells. Finally, a tennis serve can be refined using a camcorder for video feedback.
Training is social
The training process is social whether a patient works alone with a therapist or within a group. A patient’s relationship with the therapist may be the most critical aspect of training. In the context of complexity theory, models can be powerful attractors.
Taub reported a person effect when teaching handwarming. A warm, confident trainer successfully taught 20 of 21 subjects to raise their finger temperature. In contrast, an impersonal trainer only succeeded with 2 of 22 subjects. The interpersonal dynamics that make psychotherapy successful are equally important in biofeedback training.
Therapists should be credible models
Unlike stereotypical “out-of-shape” coaches with “beer guts,” biofeedback therapists have to develop and practice the skills they are teaching. Peper (1994) strongly argued that therapists must be “selfexperienced.” Would you be confident with a therapist who looked “stressed out” and extended an ice-cold handshake?
Therapists learn to self-regulate so they can model self-regulatory behaviors (like low arousal), personally know that training works, and understand their patients’ learning experiences. Since modeling involves implicit learning, a therapist who sits tensely or breathes rapidly may inadvertently teach these behaviors to a patient.
Therapists should be good coaches
An effective biofeedback therapist is a good coach. As in athletic coaching, successful biofeedback training requires clear goals, graduated rewards for success, sufficient time and practice for mastery, effective instructions delivered using systematic training techniques, useful feedback about performance, and practice of skills outside of the clinic.
Patient motivation is complex
Patient motivation is often complex and may involve the same approach-avoidance and avoidance-avoidance conflicts seen in psychotherapy.
A patient has an approach-avoidance conflict when aversive symptoms are also advantageous (gaining professional and family attention, control over relationships, and financial compensation). The rewards of symptomatic behavior are called secondary gains.
An avoidance-avoidance conflict exists when symptoms are unpleasant and biofeedback training is negatively perceived due to financial cost, time investment, or social stigma.
Finally, as in psychotherapy, significant others may sabotage training to maintain their existing relationship. This is particularly a problem in co-dependent relationships.
Assess and modify your patient’s motivation
You can assess and modify motivation by focusing on the symptoms that concern your patients. R. Adam Crane asks his patients during assessment to select three symptoms they want to improve. The patients are then asked to chart these symptoms daily throughout the course of biofeedback training. His criteria for success are a 25% to 35% decrease in symptom frequency and severity.
This protocol increases patient motivation three ways. First, involving patients in treatment decisions increases their commitment. Second, involving patients in treatment decisions and assigning responsibilities places them in an active role and increases perceived self-efficacy. Third, daily charting of symptoms should produce improvement on its own, independent of skill mastery.
Patients should be active participants
Successful patients are active participants in this leaning process. A therapist has an opportunity to modify patient expectations about their role in biofeedback training through educational literature, the assessment process, and initial training sessions.
Models that emphasize active skill learning, like Shellenberger and Green’s mastery model, may produce better clinical outcomes than those that promote passivity.
Practice determines patient success
Research indicates that patients succeed if they only practice self-regulation skills occasionally. Why is practice crucial to patient success? Practice helps a patient acquire skills through more time on task. If a patient trains 1 hour a week in the clinic, this leaves 167 hours available outside the clinic to refine skills learned during the training session.
Practice helps a patient transfer self-regulation skills to environmental settings. Handwarming in the clinic does not automatically generalize to driving in rush hour traffic. Unless a patient practices these skills in the settings where she needs them, she might only be symptom-free in the clinic.
Finally, practice makes self-regulation automatic. For example, when you learn to drive a manual transmission, you start out concentrating intensely on shifting, afraid that you will “strip the gears.” After months of practice and several gear boxes, you shift without attention. Likewise, patients practicing Stroebel’s Quieting Response perform this skill automatically after about 6 months.
Biofeedback training should teach voluntary control
Successful biofeedback training teaches voluntary control. Voluntary control is shown when a person can produce a requested physical change (warm your hand to 95 degrees F) on command without external feedback.
Voluntary control is achieved through passive and active volition. Passive volition means allowing your body to perform instead of trying to force it. Forcing defeats your purpose when trying to urinate during intermission in a movie theater, having an erection, or in Zen archery.
Active volition means forcing your body. This is used in conjunction with passive volition in modern versions of Jacobson’s Progressive Relaxation where patients are instructed to intentionally contract and relax muscle groups to detect and reduce residual muscle tension.
Despite identification of biofeedback training with passive volition, voluntary control actually involves flexibly shifting between these modes as required.
Patients should use the strategies that work for them
Schultz, who developed Autogenic Training, believed that imagery is the language the body best understands. He contended that an image serves as a blueprint for physiological change.
Research on successful self-regulators has shown that they use diverse strategies, including pictures, sounds, bodily sensations, feelings, and abstract concepts. You should encourage your patients to experiment with different strategies and then use the ones that work. This communicates respect for them as collaborators and increases their perceived self-efficacy.
Treatment protocols should incorporate current clinical findings
Both your conceptualization of a disorder and treatment design should be guided by the clinical literature. This can be frustrating for a clinician when research findings contradict conventional wisdom about a disorder. The discredited sympathetic arousal model of Raynaud’s disease provides an excellent example.
The sympathetic arousal model asserts that stressors are powerful triggers for Raynaud’s attacks and that interventions that lower sympathetic arousal will reduce symptom severity. Therapists who subscribe to this model usually provide biofeedback to lower sympathetic tone and teach stress management skills.
Research by Freedman and colleagues has challenged the sympathetic arousal model’s assumptions. Raynaud’s disease appears to be due to a “local fault” in peripheral blood vessels. Cold and cold-related stimuli are more likely to trigger vasospastic attacks than stressors. Temperature biofeedback does not produce prevent attacks by reducing sympathetic arousal. Finally, bidirectional temperature biofeedback with cold challenge produces greater symptom reduction than stress management techniques.
Failure to revise our models and treatment strategies may seriously reduce our clinical effectiveness.
Treatment protocols should be personalized
Patients reporting a symptom, like hypertension, may have very different psychophysiological profiles. Treatment should be personalized to correct abnormalities: values that are too high, low, show excessive or insufficient variability, or recover too slowly.
Biofeedback training of astronauts to reduce motion sickness during space flights illustrates this approach. A therapist monitors an astronaut’s biological systems during stress testing in a centrifuge and identifies the systems that respond abnormally. In an actual case, the major abnormality was increased skin conductance.
The therapist then designs a personalized training program to normalize the astronaut’s simulator performance. Research shows that correcting abnormalities in the simulator reduces the risk of motion sickness in space.
Personalizing treatment also means training patients to mastery criteria. For example, you might provide temperature training until your patient can achieve 95 degrees F without feedback. This is more flexible than limiting training to five sessions of temperature biofeedback whether the patient has succeeded or not. Patients have different learning curves and learning styles.
Bidirectional training may produce the best outcomes
Bidirectional training is often more effective than training in a single direction. This advantage may result from increased training time, higher proficiency standards, and learning to control more than one physiological mechanism.
Bidirectional training has been advocated in both temperature and EEG biofeedback. When teaching patients to handwarm to prevent Raynaud’s episodes, you might teach handwarming and cooling in the same or successive sessions. In neurofeedback training to control pain by increasing theta activity, ON-OFF-ON protocols (theta increase-theta suppression-theta increase) may produce the best results.
Explaining biofeedback to your patients
How do you explain biofeedback to your patients? Biofeedback metaphors help define your patient’s role in the training process. I recommend two metaphors that portray biofeedback as a process that teaches the patient skills using information about personal performance.
“Biofeedback is like coaching a runner using a stopwatch.” This metaphor emphasizes the importance of coaching in improving patient performance. “Biofeedback is like teaching carpentry, not hammering.” This metaphor communicates that the purpose of biofeedback training is to teach self-regulation instead of the mastery of a particular technique.
LEARNING CHECK
Pass your cursor over your answer. The correct answer will “glow.”
- Biofeedback training is most like
- Learning to play the piano
- Resting during lunch break
- Running a marathon
- Taking medication
- Active volition is illustrated by
- Allowing
- Experiencing
- Permitting
- Typing
- In biofeedback training, we recommend
- Massed Practice
- Negative Practice
- Spaced Practice
- 100% reinforcement
- The best way to describe the feedback a patient receives about her biological performance is
- hypnotic
- Information
- Reinforcing
- Relaxing
- The concept of biofeedback comes from ______ theory.
- Chaos
- Complexcity
- Cybernetic
- Systems
ASSIGNMENT 2
Now that you have completed this module, write down your favorite biofeedback metaphor. Based on your own clinical experience, what would you add to the discussion of the training process?
REFERENCES
Carlson, J. G., Seifert, A. R., & Birbaumer, N. (Eds.). (1994). Clinical applied psychophysiology. New York: Plenum Press.
Schwartz, M. S. (Ed.). (1995). Biofeedback: A practitioner’s guide. New York: The Guildford Press.
Shellenberger, R., & Green, J. A. (1986). From the ghost in the box to successful biofeedback training. Greeley: Health Psychology Publications.
Wickramasekera, I. A. (1988). Clinical behavioral medicine: Some concepts and procedures. New York: Plenum Press.




